
Digital Interventions for Older Adults Will Create an Alternative to Nursing Homes
Given a choice between care in a family setting and care in a nursing home, most older people prefer to maintain control and independence and choose to remain in their own home. And when it is time to decide among a variety of interventions, most will opt for approaches that are the least expensive, least medicalized, and most consistent with their earlier life. Increasingly, interventions in the environment can provide the assistance needed for older people to live safely at home for much longer than has ever been possible, and new interventions are being developed all the time.
Interventions that change a condition and improve an outcome are not confined to medicine. For instance, installing grab bars in the bathroom is an intervention, as is using a telephone that connects to one’s hearing aids. The more accommodating the environment, the less assistance it takes for the person to maneuver in it. When frailty occurs, if the person is able to overcome the effects of disability, he or she can maintain a living situation for a longer period of time, and will need less assistance than would have been the case otherwise. Unfortunately, healthcare providers often are not aware enough of nonmedical interventions and do not provide guidance to their patients to seek them out.
In the Industrial Age, assembly-line economies of scale made it less expensive to build nursing homes that delivered factory-style care than to provide individual care settings for every person who needed assistance. Digital technology has reversed that. The economies of scale and efficiencies of the assembly-line system have been overwhelmed by diseconomies of scale, building costs, and the burdensome, repetitive tasks imposed on the institutional staff. At the same time, many are questioning the assumption that older people will inevitably have to leave their homes to move into congregate settings. Digital networks equipped with sensors, screens, and audio will reduce the need to concentrate older adults in one place unless they are bed bound or have severe dementia or other mental illness. Some rural areas may not have adequate access to networks right away, but for much of the United States, monitoring can be remote and largely automatic. Attendants will not need to be present except when necessary.
Staying at home is rapidly becoming the much less expensive alternative, as well as the most desirable. New interventions are continuously remodeling the environment for older people. Innovations that have real impact change both the way the individual functions as well as reduce or change his or her service needs. For instance, a lighter wheelchair with a smaller turning radius not only reduces the square footage necessary in a bathroom, but it can relieve a homecare aide of transferring a person to the toilet because that person can now get close enough to transfer him- or herself. It also allows the person in the wheelchair to extend his or her repertory of tasks, resulting in increased exercise and emotional self-worth. As the wheelchair becomes less obtrusive, the person presents more normalized responses to the world and engages more fully in social interactions, which has enormous emotional and psychological benefits.
When interventions are successful, they become an unconscious extension of ourselves into the external world. Consider how comfortable many of us have become with the backup camera in our cars—we may forget that we used to crane our necks many times a day. It’s no wonder that this cascade of interventions, coming from almost every angle, competing and setting up new opportunities for ever-newer interventions, is too ubiquitous to be visible.
As we develop more interventions, we are slowly coming to realize that many of the conditions we assumed were an unavoidable part of aging can actually be mitigated. The position of control in aging has moved from protected environments such as nursing homes to places and services that cater to the individual’s wishes and respond to his or her directives, and to the person him- or herself. Older adults now have more resources available to them to shape their own destinies by selecting the interventions that work best for them. The fact that many frail older adults are making consumer choices, and that the market is responding to them, has transferred a portion of their care back into their own hands.
The question for those of us who work in the aging services industry is, how can we harness the capabilities we already have to further support their ability to live more and more independent, engaged, and vibrant lives?
This post was excerpted and adapted from Aging Forward: A New Path for Health, Technology, and Community by David Dunkelman and Martha Dunkelman, copyright © 2023 by Health Professions Press.
Read the book
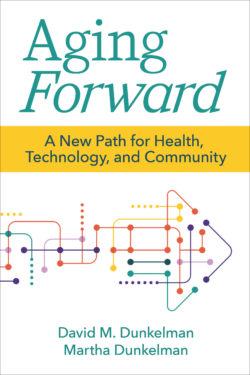 Aging Forward
Aging Forward
A New Path for Health, Technology, and Community
By David Dunkelman, J.D., M.S., and Martha Dunkelman, Ph.D.
Copyright © 2023 by Health Professions Press
America has an aging challenge. As baby boomers enter advanced age, the shortfalls of our current care delivery systems are increasingly clear. If nothing changes, we are woefully unprepared for a world with more older adults than ever before. Aging Forward confronts this inconvenient reality and provides a life raft—a vision for the future with achievable solutions.

Add comment